
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 30 August 2022
Sec. Pediatric Infectious Diseases
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.925638
 Bedasa Taye Merga1
Bedasa Taye Merga1 Gelana Fekadu2
Gelana Fekadu2 Temam Beshir Raru1
Temam Beshir Raru1 Galana Mamo Ayana1
Galana Mamo Ayana1 Fila Ahmed Hassen1
Fila Ahmed Hassen1 Miressa Bekana3
Miressa Bekana3 Belay Negash1*
Belay Negash1* Bajrond Eshetu2
Bajrond Eshetu2 Abdi Birhanu3
Abdi Birhanu3 Gutema Mulatu4
Gutema Mulatu4 Bikila Balis2
Bikila Balis2Background: Globally, newborn deaths have declined from 5 million in 1990 to 2.4 million in 2019; however, the risk of death in the first 28 days is high. Harmful umbilical cord care contributes to neonatal infection, which accounts for millions of neonatal deaths. This study assessed determinants of potentially harmful traditional cord care practices in Ethiopia using data from a nationally representative survey.
Materials and methods: Secondary data analyses were employed using data from the 2016 Ethiopian Demographic and Health Survey. Weighted samples of 4,402 mothers who gave birth in the last 3 years prior to the survey were included in the analysis. Binary logistic regression was fitted to identify associations of outcome variables with explanatory variable analysis, and the results were presented with an adjusted odds ratio (AOR) at a 95% confidence interval (CI), declaring statistical significance at a p-value < 0.05 in all analyses.
Results: About 13.70% (95% CI: 12.7%, 14.7%) of mothers practice harmful traditional umbilical cord care. Maternal age (25–34 years, AOR = 1.77, 95% CI: 1.36, 2.31, 35–49 years, AOR = 1.53, 95% CI: 1.07, 2.19), maternal education (primary: AOR = 0.54, 95% CI: 0.41, 0.70 and secondary and above: AOR = 0.61, 95% CI: 0.40, 0.94), parity (para two, AOR = 0.71, 95% CI: 0.55, 0.92), and place of delivery (home delivery, AOR = 1.96, 95% CI: 1.51, 2.56) were factors associated with potentially harmful traditional umbilical cord care practices.
Conclusion: Maternal educational status, parity, maternal age, and place of delivery were associated with harmful traditional cord care practices. Thus, improving mothers’ education, strengthening antenatal and postnatal care (PNC), and utilization of institutional delivery would help to reduce harmful traditional cord care practices.
Globally, the number of newborn deaths has declined from 5 million in 1990 to 2.4 million in 2019, however, children face the greatest risk of death in their first 28 days (1). Harmful umbilical cord care practices can directly contribute to neonatal infection, which accounts for millions of annual neonatal deaths (2, 3). Neonatal sepsis and mortality remain high in developing countries where a harmful cord care practice is high (2, 4). Africa accounts for more than 79% of the total burden of neonatal deaths worldwide (5), with neonatal deaths of 27/1,000 live births (1, 4).
Ethiopia has a relatively high neonatal death and under-5 death scores despite striving for sustainable development goals, which calls for ending preventable deaths of newborn babies and children younger than 5 years by 2030 (6). In 2019, Ethiopia ranked fourth among the countries with high neonatal mortality next to India, Nigeria, and Pakistan (1). Neonatal mortality rate in Ethiopia is 33 deaths per 1,000 live births (7). Ethiopia needs effective health measures to improve neonatal mortality to achieve the sustainable development goal (SDG) target of 12 deaths per 1,000 live birth (6).
In Ethiopia, two-thirds (66.7%) of the babies are born at home (8). In Ethiopia, severe infection is one of the top three causes of newborn death (9). National Strategy for Newborn and Child Survival has identified chlorhexidine (7.1% chlorhexidine digluconate aqueous solution or gel, delivering 4% chlorhexidine) for cord care as one of the high impact interventions to reduce the high neonatal mortality. The use of chlorhexidine, especially in setting with poor hygiene, is set as a crucial strategy to prevent life-threatening sepsis and cord infections and to avert preventable neonatal deaths in Ethiopia (10).
A neonate’s umbilical cord care is crucial in the early stage of life, and poor umbilical cord care practices have been related to infections (11). Cord infection may be confined to the umbilical cord (Omphalitis) or enter the bloodstream and become systemic (12). With standard care, the cord usually falls off between 5 and 15 days after birth. Where clean cord care is not practiced, the cord is colonized and infected by pathogenic organisms (13).
Regardless of whether the birth has taken place at home or at the health facility, substances are applied to the cord stump of the neonate; if the delivery occurred at the health facility, a substance would be placed on the cord when the infant was brought home (10). Studies from Nepal and India showed that the application of substances on the cord stump of the neonate is significantly correlated with an increased risk of omphalitis and neonatal sepsis (14, 15).
The World Health Organization (WHO) recommends the daily application of 4% chlorhexidine (7.1% chlorhexidine digluconate aqueous solution or gel, delivering 4% chlorhexidine) to the umbilical cord stump in the first week after birth only in settings where harmful traditional substances (e.g., animal dung) are commonly used on the umbilical cord (16).
However, many pieces of evidence from Ethiopia and other low-and middle-income countries have shown that mothers apply substances, such as butter, hot fermentation, lantern wax, fish bone, toothpaste, ash, charcoal, oils, vaseline, saliva, red sand, menthol-containing balm, traditional medicine, and cow dung (3, 11, 17–25). These practices often take place under unsterilized conditions; hence, they increase the risk of umbilical infection and neonatal tetanus. In Ethiopia, there is no study done on a national level on harmful traditional cord care practices. The study aimed to determine the predictors of potential harmful cord care practices among mothers in Ethiopia.
This study was conducted in Ethiopia, which is located in the horn of Africa. The country has nine regions [Afar; Tigray; Amhara; Oromia; Somali; Southern Nations, Nationalities, and People’s Region (SNNPR); Benishangul-Gumuz; Gambella; and Harari] and two administrative cities (Addis Ababa and Dire Dawa).
The study utilized data extracted from the 2016 Ethiopian Demographic and Health Survey (EDHS). Ethiopian Demographic and Health Survey collected data on basic health, demographic, and socioeconomic indicators across the nine administrative regions and two city administrations. The survey was conducted by the Central Statistical Agency (CSA) together with the Ministry of Health (MoH) and the Ethiopian Public Health Institute. The United States Agency for International Development (USAID) funded the survey. The data collection period was from 18 January 2016 to 27 June 2016 (26).
A total of 16,583 eligible women were included in the survey, 15,683 women (15–49 years) completed the interview (26). We extracted data of all mothers who gave birth in the last 3 years prior to the survey. All mothers who gave birth to alive neonates were included. Weighted samples of 4,402 mothers were included in the final analysis. Details about the DHS sampling techniques and sample size are available at http://www.dhsprogram.com/.
Any substances applied to the cord except for 4% of chlorhexidine are considered potentially harmful substances (16).
This study included sex of the child (male and female), maternal education (no education, primary education, secondary, and higher education), age of the mother (15–24, 25–34, and 35–49 years), place of residence (urban and rural), and employment status (employed and unemployed), the number of the antenatal clinic (ANC) visits was also categorized into no ANC visits, 1–3 ANC visits, four or more ANC visits, and places of delivery (categorized as a health facility or home). Parity was also categorized into para one, para two, para three, or more.
In this study, the 11 regions of Ethiopia were categorized into three contextual regions: pastoralist, agrarian, and city (which were defined on the basis of the socioeconomic and cultural backgrounds of their populations) (27).
Wealth indexes (categorized as poorest, poorer, middle, richer, and richest) were used to indicate a household’s wealth status. The wealth index was constructed using data on a household’s ownership of selected assets, such as television and bicycles, materials used for housing construction, and types of water access and sanitation facilities (26).
Analyses were performed using STATA version 14. Descriptive statistics, such as frequency and proportion, were used to describe the characteristics of the data. To assess the association between explanatory variables and potentially harmful umbilical cord care practices of mothers with children aged 0–12 months, a binary logistic regression model was fitted. First, each variable was entered into a binary logistic regression model. Second, variables, which were significant at a p-value of less than or equal to 0.25, were fitted into a multivariable logistic regression model to identify independent factors of harmful umbilical cord care practices among mothers with children aged 0–12 months in Ethiopia. Statistical significance was declared at a p-value < 0.05 in all analyses. The results from the logistic regression analyses are presented as adjusted odds ratios (AORs) with 95% confidence intervals (CIs).
A total of 4,402 mothers were included in the analysis. More than half (52.94%) of the mothers were in the 25–34 years of age group. Regarding the religion of the mothers, Muslim followers account for a major part (48.47%) followed by Orthodox (29.79%). Three-fifths (63.94%) of the respondents had no formal education, and 88.76% were from the agrarian region. The ratio of male to female children was almost 1:1. Urban resident accounts for majority of the respondents (89.99%). One out of four (25.28%) was found in the poorest wealth index (Table 1).
Almost one out of three (33.96%) mothers received all ANC visits whereas an equal proportion did not take ANC visits. Regarding mode of delivery, the majority (97.78%) gave spontaneous vaginal delivery and 71.80% gave birth at home (Table 2).
In this study, 13.70% (95% CI: 12.7%, 14.7%) of mothers applied non-medically approved substances on newborns’ umbilical stump. Of the total substances they applied, the most common were any type of oil (72.70%), ointments (17.09%), ash (1.97%), and dung (0.29%; Table 3).
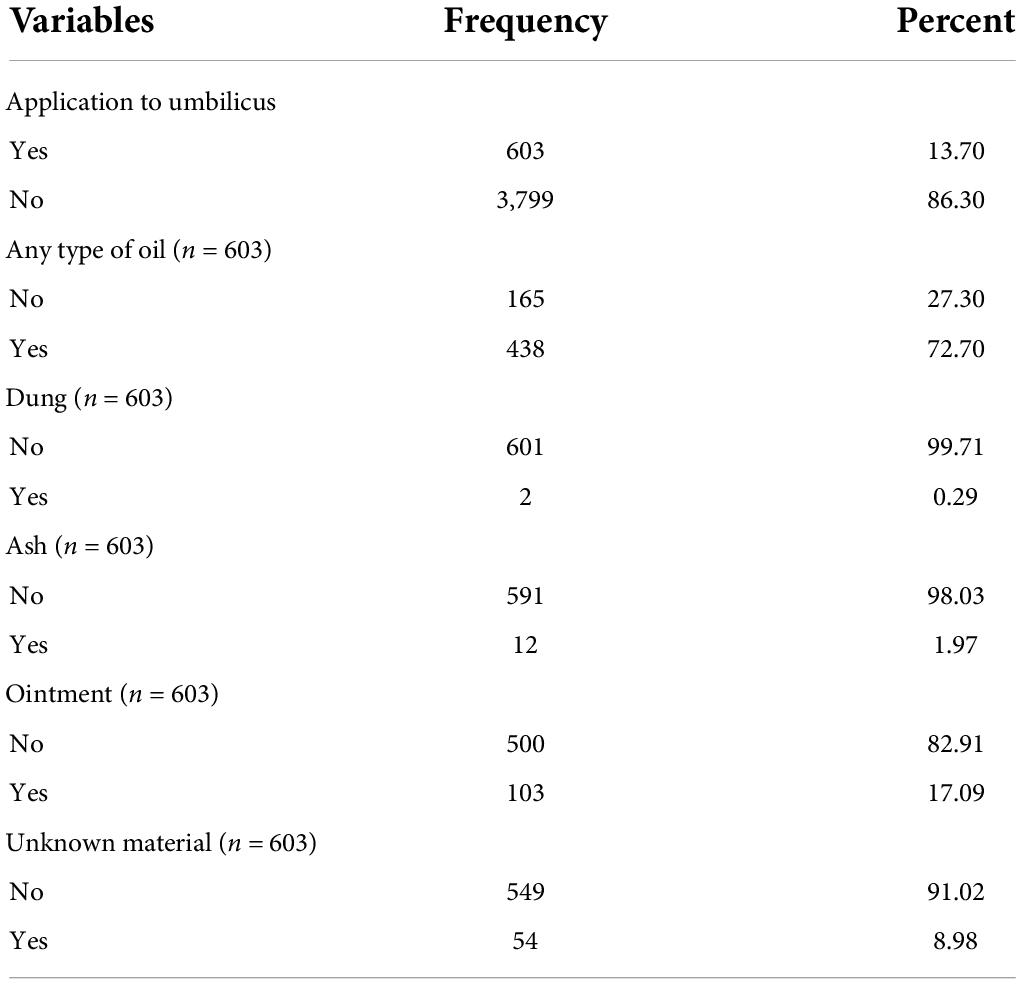
Table 3. Potentially harmful traditional umbilicus cord care practice among postnatal mothers in Ethiopia, 2016.
In bivariate logistic regression, place of residence, maternal age, maternal educational level, place of delivery, parity, wealth index, and ANC visits were factors significantly associated with potentially harmful cord care practices.
However, in multiple logistic regressions, maternal age ranging from 25 to 34 years was 1.77 times (AOR: 1.77, 95% CI: 1.36, 2.31) and age ranging from 35 to 49 was 1.53 times (AOR: 1.53, 95% CI: 1.07, 2.19) more likely to be associated with harmful traditional cord care practices. In contrast, mothers who had primary education were 0.54 times (AOR: 0.54, 95% CI: 0.41, 0.70) and secondary and above educational levels were 0.61 times (AOR: 0.61, 95% CI: 0.40, 0.94) less likely to be associated with harmful traditional cord care practices, respectively. Similarly, para two mothers were less likely to be associated with harmful traditional cord care practices as compared to mothers with less than two para (AOR: 0.71, 95% CI: 0.55, 0.92). Mothers who gave birth to their last child at home were almost two times more likely to be associated with harmful traditional cord care practices (AOR: 1.96, 95% CI: 1.51, 2.56) (Table 4).
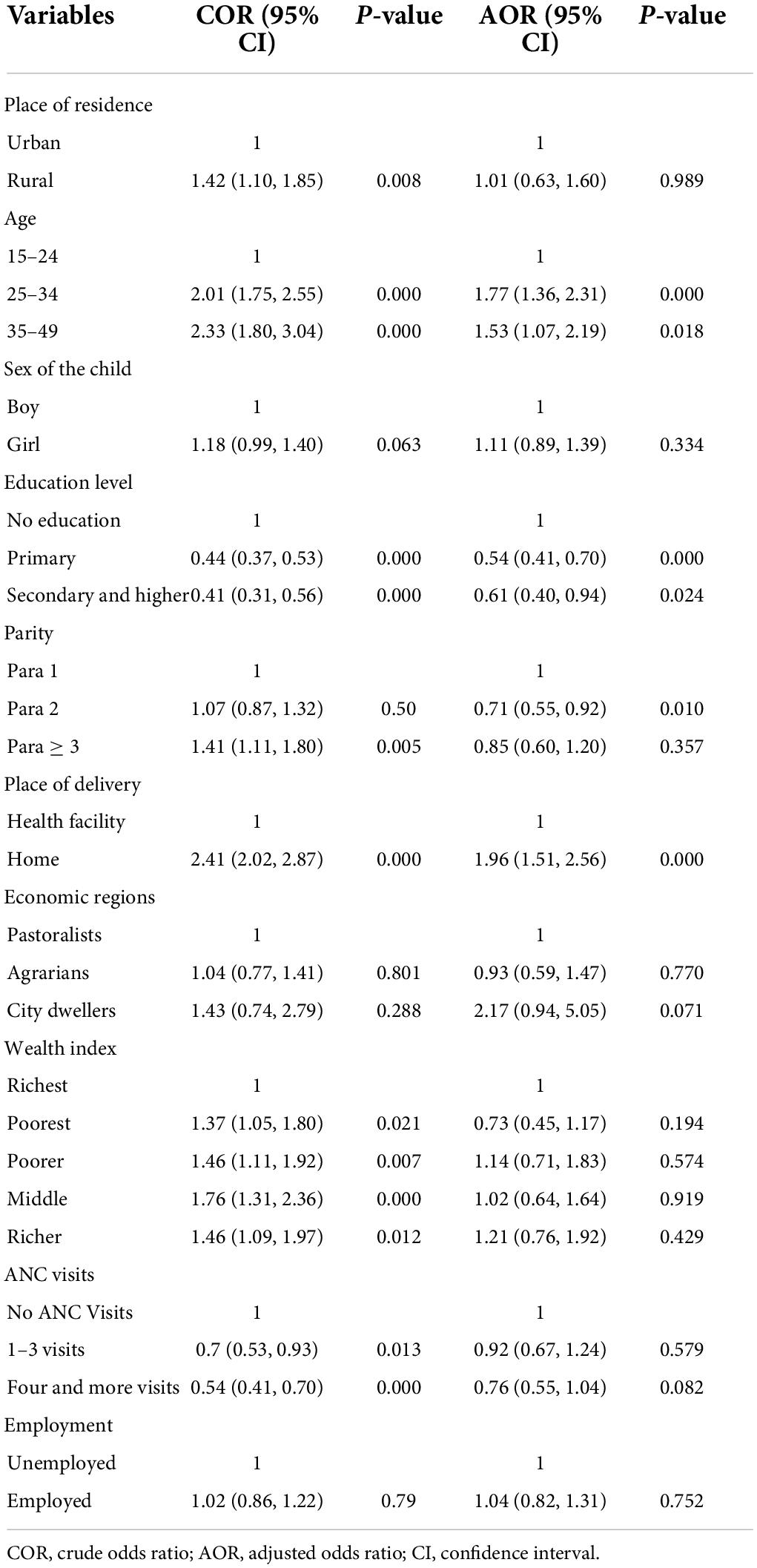
Table 4. Predictors of potentially harmful traditional cord care practices among postnatal mothers in Ethiopia, 2016.
This population-based cross-sectional survey provides factual insights regarding the determinants of potentially harmful traditional cord care practices in Ethiopia. This study revealed that more than one in eight mothers applied substances not medically recommended, which potentially increases the risk of cord infection. The practices of applying traditional substances to the cord stump in Ethiopia call for actions that increase antenatal care, delivery services, and postnatal care (PNC) utilizations where both mothers and newborns are benefited. Clean, dry cord care is recommended by WHO for newborns in health facilities and at home in low neonatal mortality settings. The use of chlorhexidine in these situations may be considered only to replace the application of a harmful traditional substances, such as cow dung to the cord stump (16).
In this study, 13.70% of mothers applied potentially harmful substances, such as dung, oil, ointments, ash, and butter on the umbilical stump of the neonates. This finding was lower than the studies done in Benin City (46.1%) (17), Nigeria (22.2 and 67.3%) (18, 19), Nepal (26 and 43%) (28), Uganda 39.6% (3), Southwest Ethiopia (20.4 and 54.7%) (20, 23), and Eastern Ethiopia (29.3%) (24). The discrepancy may be due to variations in access to awareness, geographical variations, and health-seeking behavior across the different cultural beliefs. This has health implications for newborns’ infection and tetanus (29–32).
The maternal ages ranging from 25 to 34 and from 35 to 49 years were positively associated with harmful traditional cord care practices as compared to the maternal age ranging from 15 to 24 years. This is supported by a study done in Nigeria (18). The possible justification might be that the older mothers were less likely to adhere to ANC visits, skilled birth attendants, and PNC visits, which help them to get counseling from care providers on recommended cord care practices. In addition, older mothers learn or are influenced by society who might not always be the source of the correct information and the belief that applying substances could help facilitate fast healing (19, 20).
Mothers with primary education and secondary/above had lower odds of application of potentially harmful substances to the stump of the umbilical cord when compared with mothers with no formal education. These findings are consistent with studies that show the positive associations between a higher level of maternal education and better health-seeking behavior and thus medically recommended child cord care practices (7, 20).
Similarly, in our study, we found that mothers who gave birth two times revealed a large reduction in the odds of practicing potentially harmful traditional cord care. This is due to the fact that mothers who have exposure to childbirth have a chance to get clean cord care information from health care providers (33–36). This can be explained by mothers having previous experience of delivery and obtaining information about essential newborn care during their previous ANC, delivery, PNC, and immunization periods, and this can inspire mothers to practice essential newborn care more.
Mothers who delivered their last child at home had higher odds of practicing potentially harmful traditional cord care as compared to those who delivered at a health institution. The reason for this could be the fact that mothers who gave birth at home may be influenced by social customs or were unaware of the health risks involved related to the application of potentially harmful substances to the stump of the umbilical cord (11, 37). When the birth is at the relatives, traditional birth attendants or neighbors may apply substances to the umbilicus of the newborn (34). In contrast, mothers who gave birth at the health facility were more likely to receive ANC, which creates an opportunity to counsel mothers about recommended newborn cord care practices and to be aware of risks of infection related to the application of harmful substances on the stump of the umbilical cord (28, 38). This implies that pregnant women need ANC, skilled birth attendants, and postpartum care to promote better newborn care practices, specifically hygienic cord care.
The study utilized data from a nationally representative survey, which could be considered a strength. However, this study was not without limitations. Harmful traditional substances applied on the umbilical stump of the newborns were a self-reported event by the mother/caregiver, which may result in recall bias. The data provided the proportion of women who applied anything to the cord stump and some substances, which are potentially harmful; however, the data did not present the proportion of 4% chlorhexidine applied to the stump, which is recommended by WHO. The other limitation is that the cross-sectional study design cannot establish a temporal relationship between the outcome and response variables.
A significant proportion of women practice harmful traditional cord care in Ethiopia, and multifaceted factors appear to determine their practices. Maternal educational status, parity, maternal age, and place of delivery were independently associated with harmful traditional cord care practices. Thus, intervention strategies that emphasize primipara and older women to practice safe umbilical cord care may halt the problem. Moreover, improving the educational status of women and utilization of institutional delivery would help to reduce the prevalence of harmful traditional cord care practices.
Publicly available datasets were analyzed in this study. This data can be found here: The datasets used for analysis are available from http://www.dhsprogram.com/ up on reasonable request.
The study was ethically reviewed and approved by the National Research Ethics Review Committee (NRERC) of Ethiopia. Written informed consent was obtained from participants prior to data collection.
BB and BM: conceived and designed the study. BM, TR, GA, and GF: methodology. MB, FH, BE, and BN: analysis. BM, AB, GM, and BB: drafting the manuscript and made revisions. All authors contributed to data analysis, drafting, or revision of the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
The authors would like to express their deepest gratitude to measure DHS, ICF International, Rockville, MD, United States, for providing the data for the analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; ANC, antenatal care; COR, crude odds ratio; PNC, postnatal care.
1. World Health Organization. Newborns: Improving survival and well-being. (2020). Avaliable online at: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality (accessed December 20, 2021)
2. Mallick L, Yourkavitch J, Allen C. Trends, determinants, and newborn mortality related to thermal care and umbilical cord care practices in South Asia. BMC pediatr. (2019) 19:248. doi: 10.1186/s12887-019-1616-2
3. Turyasiima M, Nduwimana M, Andres SM, Kiconco G, Egesa WI, Maren BM, et al. Neonatal umbilical cord infections: Incidence, associated factors and cord care practices by nursing mothers at a tertiary Hospital in Western Uganda. Open J Pediatr. (2020) 10:288. doi: 10.4236/ojped.2020.102030
4. UNICEF. Neonatal mortality. (2021). Avaliable online at: https://data.unicef.org/topic/child-survival/neonatal-mortality/ (accessed December 20, 2021.
5. Hug L, Alexander M, You D, Alkema L. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: A systematic analysis. Lancet Glob Health. (2019) 7:e710–20. doi: 10.1016/S2214-109X(19)30163-9
6. United Nations. Sustainable development goals. (2015). Avaliable online at: https://www.undp.org/sustainable-development-goals. (accessed date December 15, 2021
7. Edhs M. Mini demographic and health survey. (2019). Avaliable online at: https://www.dhsprogram.com/pubs/pdf/FR363/FR363.pdf. (accessed date December 20, 2021
8. Ayenew AA, Nigussie AA, Zewdu BF. Childbirth at home and associated factors in ethiopia: A systematic review and meta-analysis. Arch Public Health. (2021) 79:48. doi: 10.1186/s13690-021-00569-5
11. Coffey PS, Brown SC. Umbilical cord-care practices in low-and middle-income countries: A systematic review. BMC Pregnancy Childbirth. (2017) 17:68. doi: 10.1186/s12884-017-1250-7
12. Chizoma MN, Fisayo Oluwatosin M, Abimbola OO. Umbilical cord care knowledge and practices of mothers attending selected primary health care centres in Ibadan, Nigeria. Int J Caring Sci. (2020) 13:143–51.
13. World Health Organization. World health organization recommendations on newborn health. (2017). Avaliable at https://www.who.int/docs/default-source/reproductive-health/stillbirth/who-mca-17-07-eng.pdf?sfvrsn=bf769add_2. (accessed December 20, 2021)
14. Goel A, Murmu SK, Shah S, Chawla GS. Role of cultural practices in neonatal sepsis. Int J Med Sci Public Health. (2015) 4:680–3. doi: 10.5455/ijmsph.2015.01012015140
15. Mullany LC, Darmstadt GL, Katz J, Khatry SK, LeClerq SC, Adhikari RK, et al. Risk factors for umbilical cord infection among newborns of southern Nepal. Am J Epidemiol. (2007) 165:203–11. doi: 10.1093/aje/kwj356
16. World Health Organization. WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization (2022).
17. Abhulimhen-Iyoha B, Ofili A, Ibadin M. Cord care practices among mothers attending immunization clinic at the University of Benin Teaching Hospital, Benin City. Niger J Paediatr. (2011) 38:104–8. doi: 10.4314/njp.v38i3.72262
18. Asma’u A, Oloche OB, Ridwan JM, Muhammad A, Mohammad AU, Omeneke IK, et al. Determinants of umbilical cord care practices among mothers of neonates admitted into special care baby unit of usmanu Dan Fodiyo University teaching hospital. Sokoto: International Journal of Contemporary Medical Research (2021).
19. Opara PI, Jaja T, Dotimi DA, Alex-Hart BA. Newborn cord care practices amongst mothers in yenagoa local government rea, Bayelsa State, Nigeria. Int J Clin Med. (2012) 3:22–7. doi: 10.4236/ijcm.2012.31004
20. Sakelo AN, Assefa N, Oljira L, Assefa ZM. Newborn Care practice and associated factors among mothers of one-month-old infants in southwest ethiopia. Int J Pediatr. (2020) 2020:3897427. doi: 10.1155/2020/3897427
21. Smith CK. Some traditional umbilical cord care practices in developing countries. Midwifery Today Int Midwife. (2009) 91:12–3.
22. Stewart D, Benitz W, Watterberg KL, Committee On Fetus And Newborn. Umbilical cord care in the newborn infant. Pediatrics. (2016) 138:e20162149. doi: 10.1542/peds.2016-2149
23. Dessalegn N, Dagnaw Y, Seid K, Wolde A. Umbilical cord care practices and associated factor among mothers of neonates visiting Mizan-Tepi university teaching hospital southwest ethiopia 2021. Pediatr Health Med Ther. (2022) 13:227. doi: 10.2147/PHMT.S363252
24. Eyeberu A, Getachew T, Debella A, Birhanu A, Alemu A, Dessie Y. Practicing Level and determinants of safe cord care and skin-to-skin contact among post-partum women in public hospitals of eastern ethiopia. Front Pediatr. (2022) 10:883620. doi: 10.3389/fped.2022.883620
25. Weldeargeawi GG, Negash Z, Kahsay AB, Gebremariam Y, Tekola KB. Community-based essential newborn care practices and associated factors among women of Enderta, Tigray, Ethiopia, 2018. Int J Reprod Med. (2020) 2020:2590705. doi: 10.1155/2020/2590705
26. Central Statistical Agency. Ethiopia demographic and health survey 2016. Addis Ababa: Central Statistical Agency (2016). 551 p.
27. EFMoH. Health System Strengthening & Special Support. (2015). Available online at: https://www.moh.gov.et/site/directorates/health-system-special-support
28. USAID. Thermal care and umbilical cord care practices and their associations with newborn mortality. (2018). Avaliable online at: https://dhsprogram.com/publications/publication-as68-analytical-studies.cfm. (accessed date December 20, 2021).
29. Getabelew A, Aman M, Fantaye E, Yeheyis T. Prevalence of neonatal sepsis and associated factors among neonates in neonatal intensive care unit at selected governmental hospitals in Shashemene Town, Oromia regional state, Ethiopia, 2017. Int J Pediatr. (2018) 2018:7801272. doi: 10.1155/2018/7801272
30. Alemu M, Ayana M, Abiy H, Minuye B, Alebachew W, Endalamaw A. Determinants of neonatal sepsis among neonates in the northwest part of Ethiopia: Case-control study. Ital J Pediatr. (2019) 45:150. doi: 10.1186/s13052-019-0739-2
31. Mir F, Tikmani SS, Shakoor S, Warraich HJ, Sultana S, Ali SA, et al. Incidence and etiology of omphalitis in Pakistan: A community-based cohort study. J Infect Dev Ctries. (2011) 5:828–33. doi: 10.3855/jidc.1229
32. Teshale AB, Tesema GA. Determinants of births protected against neonatal tetanus in Ethiopia: A multilevel analysis using EDHS 2016 data. PLoS One. (2020) 15:e0243071. doi: 10.1371/journal.pone.0243071
33. Abegunde D, Orobaton N, Beal K, Bassi A, Bamidele M, Akomolafe T, et al. Trends in newborn umbilical cord care practices in Sokoto and Bauchi States of Nigeria: The where, who, how, what and the ubiquitous role of traditional birth attendants: A lot quality assurance sampling survey. BMC Pregnancy Childbirth. (2017) 17:368. doi: 10.1186/s12884-017-1551-x
34. Amare Y. Umbilical cord care in Ethiopia and implications for behavioral change: A qualitative study. BMC Int Health Hum Rights. (2014) 14:12. doi: 10.1186/1472-698x-14-12
35. Asiedu SSO, Apatu NAA, Tetteh R, Hodgson A. Neonatal cord care practices among mothers and caregivers in the Volta region of Ghana. Int J Matern Child Health AIDS. (2019) 8:63. doi: 10.21106/ijma.272
36. Ambe J, Bello M, Yahaya S, Omotora B. Umbilical cord practices in Konduga local government area of Bornu State, North East Nigeria. J Trop Med. (2010) 9:87–92.
37. Amare Y, Degefie T, Mulligan B. Newborn care seeking practices in central and southern Ethiopia and implications for community based programming. Ethiop J Health Dev. (2013) 27:3–7.
Keywords: umbilicus cord care, harmful practice, DHS, Ethiopia, pediatric
Citation: Merga BT, Fekadu G, Raru TB, Ayana GM, Hassen FA, Bekana M, Negash B, Eshetu B, Birhanu A, Mulatu G and Balis B (2022) Determinants of potentially harmful traditional cord care practices among mothers in Ethiopia. Front. Pediatr. 10:925638. doi: 10.3389/fped.2022.925638
Received: 21 April 2022; Accepted: 29 July 2022;
Published: 30 August 2022.
Edited by:
Valeriane Leroy, Institut National de la Santé et de la Recherche Médicale (INSERM), FranceReviewed by:
Patricia S. Coffey, PATH, United StatesCopyright © 2022 Merga, Fekadu, Raru, Ayana, Hassen, Bekana, Negash, Eshetu, Birhanu, Mulatu and Balis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Belay Negash, bmVnYXNoLmJlbEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.